Over the past few decades, fertility science has advanced from the first “test-tube baby” to a bold new frontier: making eggs and sperm in the lab from ordinary cells such as skin or blood. In 1978 Louise Brown became the first baby born via in vitro fertilization (IVF). IVF today helps many infertile couples, but it still requires that one parent have viable eggs or sperm. Women who have no eggs (for example after cancer treatments) or men with no sperm have had no way to have genetically related children. The game changed when Shinya Yamanaka showed in 2007 that adult cells (like skin fibroblasts) can be reprogrammed into induced pluripotent stem cells (iPSCs) that behave like embryonic stem cells.
In theory, such stem cells could be steered to become any tissue, even sperm or egg cells. This idea spurred efforts to recreate gametogenesis in vitro, a process now called in vitro gametogenesis (IVG). Early work in mice confirmed it was possible to generate functional gametes from stem cells. In 2011 Kyoto University researchers coaxed mouse iPSCs into primordial germ cells, transplanted them into testes, and obtained sperm that produced healthy pups. By 2016, that team (Hayashi and Saitou) had carried out the entire female germ-line cycle in vitro: turning mouse stem cells into eggs, fertilising them by IVF, and deriving new embryonic stem cells, even generating a second cycle of egg production.
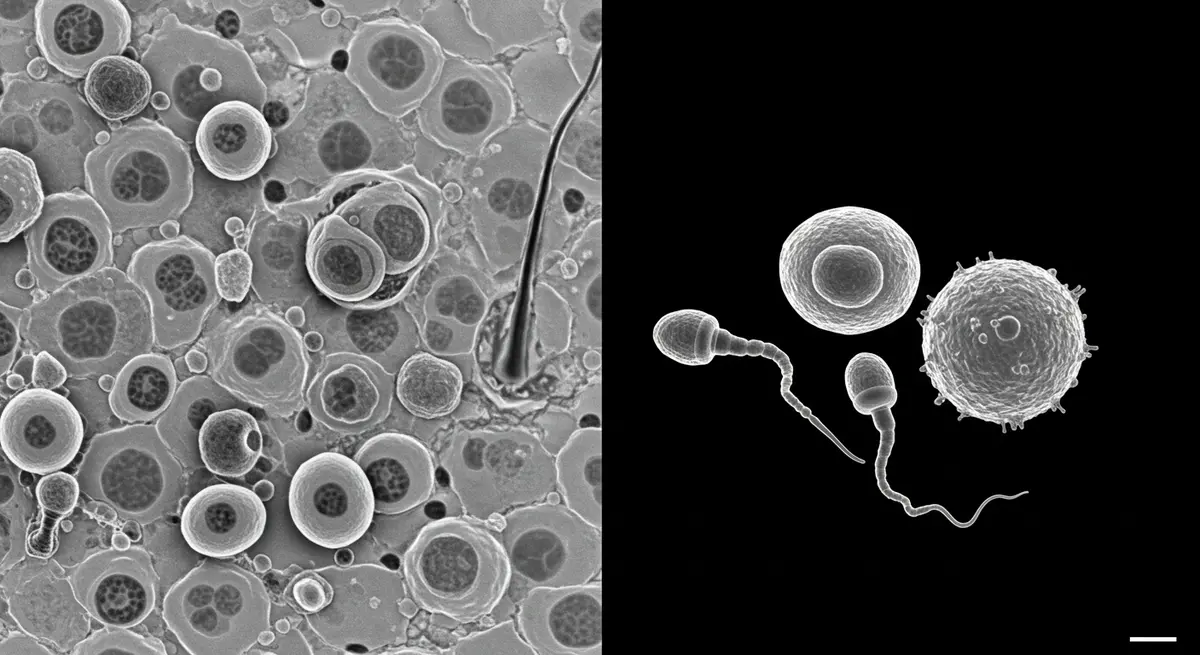
These lab-made mouse eggs and sperm were used to create normal mouse offspring. In short, for the first time scientists achieved proof-of-principle that mammalian gametes can be grown from somatic cells outside the body. (For context, note that in 1996 the same technique of transferring a body-cell nucleus into an enucleated egg was used to clone Dolly the sheep. But Dolly was a clone of one parent, whereas IVG aims to combine genetic material from two parents in a new embryo.)
Current Progress
In recent years, laboratories worldwide have made steady progress toward turning skin cells into gametes, using two main strategies. iPSC-based IVG: Many groups turn somatic cells into iPSCs and then coax them to become primordial germ cell–like cells (PGCLCs). These precursor germ cells must then be matured through meiosis to form haploid eggs or sperm. Japanese teams have led these efforts. In 2023, Katsuhiko Hayashi’s group (Kyushu University, Osaka) reported for the first time the creation of viable mouse eggs from male (XY) cells. They reprogrammed male skin cells to iPSCs, then removed the Y chromosome and duplicated an X chromosome (to mimic a female XX genome), and matured the cells in an “ovary in a dish.” When those lab-grown eggs were fertilised and implanted, about 1% of embryos developed into live mouse pups. This groundbreaking result shows same-sex (male-male) parenthood is theoretically possible in mammals. Prof. Hayashi said his lab is now attempting to apply the same process to human cells.
Another major approach skips the iPSC stage and instead uses somatic-cell nuclear transfer (SCNT). In this method, researchers take the nucleus (which contains the DNA) from a donor skin cell and transplant it into a healthy egg cell whose own nucleus has been removed. The egg’s own machinery then tricks the transplanted nucleus into halving its chromosomes – essentially performing a faux-meiosis – so that the egg becomes haploid (containing a single set of chromosomes) rather than diploid. (The process is similar to cloning Dolly the sheep, but with a twist: after the skin-cell nucleus is “haploidised” in the egg, the reconstructed egg can be fertilised by sperm from a second parent.) In 2022–24 Shoukhrat Mitalipov’s team at Oregon Health & Science University (OHSU) published detailed mouse studies of this SCNT-IVG method. They showed that mouse skin-cell nuclei transferred into eggs can indeed extrude one set of chromosomes into a pseudo-polar body upon fertilisation, yielding embryos with one chromosome set from the skin cell and one from the sperm. Roughly 16–18% of such reconstructed embryos developed to blastocysts, and importantly the researchers derived embryonic stem cell lines and even live mouse pups from them. In effect, they created healthy offspring whose mother was an egg reconstructed from a skin cell, and whose father was the sperm donor. These experiments demonstrate a concrete path to making eggs from adult cells without first generating iPSCs.
Researchers perform somatic-cell nuclear transfer in the lab. A fine pipette inserts a skin-cell nucleus into a mouse egg (whose own nucleus has been removed) under microscopic guidance. The egg’s cytoplasm then causes the transplanted nucleus to discard half its chromosomes, creating a haploid egg cell ready for fertilization. In this way the OHSU team turns a skin cell into an egg that can be fertilized and produce viable embryos.
On the human side, IVG is still at the research stage. In 2015–2016 Kyoto University researchers established conditions to turn human iPSCs into primordial germ cell–like cells. More recently, in 2024 the same group (WPI-ASHBi Kyoto) reported in Nature that they had achieved a new milestone: driving human PGCLCs further along the germline path to mitotic oogonia and prospermatogonia stages by using specific signaling cues. These oogonia-like cells behaved much like very early fetal germ cells (showing correct gene expression and DNA reprogramming) and could be multiplied billions-fold in culturen. This advance brings scientists closer to eventually completing human gametogenesis in a dish. Parallel efforts in the U.S. include a Silicon Valley startup, Conception Biosciences, backed by investors like OpenAI’s Sam Altman. Conception aims to turn adult cells into egg cells, and its CEO has suggested lab-grown eggs could become a powerful tool (for example, to counter declining birth rates or to enable gene-editing of the human germline). Altogether, scientists in Japan, the U.S., and elsewhere are racing toward the goal of human IVG.
Global and Regional Developments
IVG research is international. Japan has been a trailblaser: Kyoto University’s Mitinori Saitou and Hayashi groups have produced much of the foundational work on stem-cell gametogenesis in mice and human cells. Professor Katsuhiko Hayashi of Osaka University continues to be a high-profile leader, and at international meetings he has predicted that human IVG (even deriving eggs from male cells) may be possible “within a decade” if safety issues are addressed. Japan’s fertility regulators have recently considered new guidelines for embryo research, but so far allow limited research on human gamete formation under strict review.
In the United States, key players include Dr. Shoukhrat Mitalipov’s OHSU Center for Embryonic Cell and Gene Therapy (focusing on SCNT-IVG), and Conception Biosciences (a biotech startup working on iPSC-to-egg technology). U.S. federal law currently prohibits transfer of lab-grown (especially genetically modified) embryos into a womb, and agencies like the FDA treat germ-cell therapies as sensitive areas, so clinical use of IVG in people is years away. However, the regulatory view is evolving: in 2025 the UK’s fertility regulator (HFEA) recommended that IVG should be explicitly regulated by law once it is safe. The HFEA noted that IVGs could “vastly increase the availability of human sperm and eggs for research and, if proved safe… to provide new fertility treatment options”, but it also cautioned that “biologically dangerous use of IVGs in treatment should never be permitted” under current law. Other countries have similar debates. In Europe, many nations allow limited embryo research (often with a 14-day rule on embryos), but the consensus is that IVG will require new policies and ethical oversight. China has a booming IVF industry but has not publicly reported any lab-made human gamete breakthroughs; a few unverified reports (e.g. claimed artificial mouse sperm in 2016) have been met with skepticism. Overall, the global trend is cautious optimism: researchers note that what has worked in mice will likely work in humans eventually but they emphasise it must be done carefully.
Key Challenges
Several major challenges remain before IVG can become a practical reality:
- Completing Meiosis: Natural eggs and sperm undergo meiosis to halve their chromosome number. Replicating this precisely in vitro is extremely difficult. In SCNT-based IVG, the egg must mimic a meiosis I division to discard exactly one copy of each chromosome. Even in Mitalipov’s mouse experiments, perfect haploidisation (with exactly one of each chromosome going into the pseudo–polar body) was rare, and mismatches can cause aneuploid embryos. In the Hayashi male-to-egg study, only about 1% of embryos from lab-made eggs yielded live pups (versus ~5% in normal IVF), highlighting low efficiency. Scientists are working to understand the subtle cellular cues that ensure correct chromosome segregation.
- Epigenetic Reprogramming: Germ cells must erase most of the DNA “memory” inherited from the parents (epigenetic marks) to become true gametes. Studies indicate that human primordial germ cell–like cells in vitro often fail to complete this reprogramming, which is essential for fertility. The Kyoto team found that adding bone morphogenetic protein (BMP) signals helped overcome some reprogramming hurdles, but robustly erasing imprints (such as DNA methylation patterns) remains a technical hurdle. Until this is solved, lab-made gametes could carry abnormal epigenetic marks, potentially causing developmental problems.
- Safety and Genetic Integrity: Any eggs or sperm made in vitro would need extensive quality control. Because IVG could introduce new mutations or epigenetic errors, embryos conceived from such gametes would likely require pre-implantation genetic screening for abnormalities. As one expert cautioned, “even with these safeguards in place… some patients would have to make a leap of faith” about residual risks. Achieving the necessary safety standards will take time.
- Ethical and Regulatory Hurdles: IVG raises difficult ethical questions. For example, generating large numbers of embryos (dozens or hundreds from one skin biopsy) could change the social context of IVF and embryo. Legal frameworks vary: many countries (like the UK) currently ban clinical use of IVG until laws are updated. The need for careful oversight is broadly recognised. The ISSCR and other bodies emphasise transparent, responsible research. Notably, the UK’s regulator has already signaled that IVGs should be tightly regulated and that any clinical use would require new legislation. As Stanford ethicist Henry Greely put it, “I don’t see any show stopper that will keep what is feasible in mice from working in humans,” but he warns that “the clinical need for such a technology is tremendous… some patients would have to make a leap of faith” about its risks.
Future Directions
Experts predict that human IVG will likely transition from mouse experiments to safe human cells over the next decade or two. Professor Hayashi and colleagues suggested that viable human IVG “could be possible within 10 years” if technical obstacles are solved. In mid-2025, Hayashi noted that his lab believes it is only a “few years” away from creating human eggs and sperm from somatic cells. Other voices urge caution; Harvard’s George Daley points out that human gametogenesis is more complex than mice and may take longer to master. In any case, the field is advancing rapidly. Laboratories will likely combine new tools (3D organoids, genome editing, high-throughput screening) to refine gamete production. Private companies are also pouring money into this “race”. Some futurists even discuss the possibility of extending IVG to create embryonic stem cells that develop entirely outside the body (along with future artificial womb technology).
Research efforts will also expand to animals. Beyond mice, teams are exploring IVG in livestock (which could revolutionise breeding) and in endangered species. For example, Hayashi’s group has begun attempting to generate eggs from skin cells of the northern white rhinoceros, which has only two living females left. If successful, IVG could allow preservation of genetic diversity by making gametes from each cell line.
Finally, IVG may merge with gene-editing. Lab-made gametes could be easily gene-edited before fertilisation, raising the prospect of correcting genetic diseases in the germline. As one commentator noted, lab-grown eggs might offer a platform for human germline engineering in the future. Policymakers and scientists agree this will require global ethical debate.
Potential Applications
If IVG becomes practical, it could transform medicine and reproduction in many ways:
- Treating Infertility: The most obvious application is helping infertile individuals. Women who have lost ovarian function (due to age, surgery, or chemotherapy) could potentially have eggs made from their own somatic cells. Men with nonfunctional testes could similarly obtain sperm from their cells. Co-author Paula Amato of OHSU notes that this could benefit “women of advanced maternal age” and others who can’t produce eggs. IVG could enable people with genetic fertility problems to have healthy, genetically related children without donor gametes.
- Same-Sex and Solo Parenthood: IVG opens the door to new family possibilities. For example, two men could have a child genetically related to both by turning one man’s skin cells into eggs and fertilising them with the other’s sperm. Likewise, two women could conceive without donor sperm. More speculatively, IVG could even allow unusual genetic combinations (some have imagined an embryo with DNA from four people, or a “unibaby” created from one person’s cells). These scenarios raise ethical debates but show the breadth of IVG’s potential.
- Disease Modeling and Research: Lab-made gametes would be valuable in research. Scientists could model inherited diseases by creating eggs or sperm carrying specific mutations, then studying early development. IVG could also yield embryonic stem cells with patient-specific genomes for studying disease or testing drugs. As one review notes, IVG “allows for exploration of germ cell development” and offers “possibilities in reproductive medicine… for disease modelling”.
- Animal Breeding and Conservation: Beyond humans, IVG could boost agriculture and conservation. Livestock breeders might use IVG to produce many gametes from a prized animal without invasive procedures. Conservationists see IVG as a way to save endangered species with very few animals remaining. Researchers at Kyoto are already applying IVG methods to make eggs for northern white rhinos. In farming, IVG could accelerate selective breeding or propagate rare genetics.
- Population and Demographic Effects: Some futurists suggest that widespread IVG could affect population trends. For instance, since women’s fertility peaks at young ages but many postpone childbearing, IVG could allow older women to have genetically related children. In fact, Conception’s CEO has speculated that lab-grown eggs might be “the best tool we have to reverse population decline”. If infertility becomes easily treatable, societies with aging populations might see birth rates rise.
In summary, turning somatic cells into gametes is a rapidly advancing field with profound implications. On the technical side, scientists have already demonstrated complete mouse gametogenesis in vitro and taken major steps in human cells. On the human side, the path is still being charted. But even now, major fertility centers and startups are investing in IVG, anticipating that one day it could let anyone – regardless of age, sex, or fertility status – have biological children. If that future arrives, IVF may no longer depend on finding a viable egg or sperm in the body, but only on taking a skin sample and growing gametes in the lab.
Sources
Reproduction revolution: how our skin cells might be turned into sperm and eggs | Genetics | The Guardian
https://www.theguardian.com/science/2018/oct/14/scientists-create-sperm-eggs-using-skin-cells-fertility-ethical-questions
Research sheds light on new strategy to treat infertility | OHSU News
https://news.ohsu.edu/2024/03/08/research-sheds-light-on-new-strategy-to-treat-infertility
The Future of Fertility | The New Yorker
https://www.newyorker.com/magazine/2023/04/24/the-future-of-fertility
Scientists create mice with two fathers after making eggs from male cells | Genetics | The Guardian
https://www.theguardian.com/science/2023/mar/08/scientists-create-mice-with-two-fathers-after-making-eggs-from-male-cells
Haploidy in somatic cells is induced by mature oocytes in mice | Communications Biology
https://www.nature.com/articles/s42003-022-03040-5?
Groundbreaking study advances human in vitro gametogenesis for infertility treatment
https://www.news-medical.net/news/20240521/Groundbreaking-study-advances-human-in-vitro-gametogenesis-for-infertility-treatment.aspx
Lab-grown sperm and eggs just a few years away, scientists say | Reproduction | The Guardian
https://www.theguardian.com/science/2025/jul/05/lab-grown-sperm-and-eggs-scientists-reproduction
The HFEA’s recommendation to government on the future regulation of in-vitro gametes | HFEA
https://www.hfea.gov.uk/about-us/news-and-press-releases/2025/the-hfea-s-recommendation-to-government-on-the-future-regulation-of-in-vitro-gametes/
Modelling in vitro gametogenesis using induced pluripotent stem cells: a review | Cell Regeneration
https://cellregeneration.springeropen.com/articles/10.1186/s13619-023-00176-5